Alzheimer’s disease research is rapidly evolving, shedding light on the mechanisms behind one of the most common neurodegenerative diseases today. Central to this research is the study of microglial cells, which function as the brain’s immune system, patrolling and responding to potential threats. Recent breakthroughs in understanding how these cells operate, particularly through the work of Beth Stevens, have unveiled critical insights into the role of faulty synaptic pruning in Alzheimer’s development. By identifying biomarkers for Alzheimer’s, researchers can potentially intervene much earlier in the disease process, offering hope to millions. As the demographics of our population shift, the importance of such research cannot be overstated, with predictions of increased incidence only amplifying the urgency for innovative treatments.
Exploring the complexities of Alzheimer’s disease, a condition characterized by cognitive decline and memory loss, highlights the pressing need for advancements in understanding its underlying biological mechanisms. This investigation into the brain’s immune response involves key players such as microglial cells, which are pivotal in maintaining neurological health through their surveillance activities. Research spearheaded by experts like Beth Stevens showcases how irregular functioning of these immune cells contributes to broader issues in neurodegenerative disorders. By focusing on the discovery of specific biomarkers for Alzheimer’s, scientists aim to enhance early detection and intervention strategies. Consequently, this expanding knowledge base is not only crucial for improving individual lives but also for addressing the growing public health challenge associated with aging populations.
The Role of Microglial Cells in Alzheimer’s Disease
Microglial cells are essential components of the brain’s immune system, playing a pivotal role in maintaining overall brain health. These cells are responsible for monitoring the brain’s environment, removing dead neurons, and participating in synaptic pruning—an essential process for normal brain function. However, recent research indicates that dysfunction within microglial cells can lead to neurodegenerative diseases, including Alzheimer’s. As the work of Beth Stevens shows, microglial cells can become overactive or misdirected, contributing to the progression of neurodegenerative conditions. This insight into the behavior of microglia opens new avenues for potential therapeutic interventions.
Understanding the dynamics of microglial cells holds promise for identifying biomarkers for Alzheimer’s disease. Stevens’ research emphasizes the need for early detection methods that can pinpoint when microglial overactivity occurs and how it correlates with the onset of Alzheimer’s symptoms. By analyzing these immune cells, scientists hope to detect the earliest signs of neurodegeneration, potentially allowing for earlier treatment options. Ultimately, by comprehending the complexities of microglial behavior, researchers aim to establish a clearer connection between these immune cells and neurodegenerative diseases, leading to innovative approaches in dementia care.
Discoveries in Neurodegenerative Diseases
Neurodegenerative diseases such as Alzheimer’s disease and Huntington’s disease pose significant challenges for healthcare systems worldwide. The groundbreaking research conducted by Beth Stevens highlights how the failure of microglial cells in their cleaning and support roles can exacerbate these conditions. Stevens’ work showcases the intricate relationship between the brain’s immune system and neurodegeneration, underscoring how critical interventions might stem from a deeper understanding of these cellular processes. This approach could lead to new therapeutic strategies aimed at restoring the normal function of microglial cells, thereby potentially halting or even reversing the progression of neurodegenerative diseases.
The implications of Stevens’ findings extend beyond basic research; they suggest a paradigm shift in how we approach Alzheimer’s treatment. By discovering specific biomarkers for Alzheimer’s disease within the actions of microglial cells, researchers might be able to develop targeted therapies that modulate immune responses to better protect neuronal health. Moreover, as the population ages, the necessity for effective treatment options becomes increasingly urgent. Stevens’ explorations provide a hopeful outlook, showing that advances in understanding the cellular mechanisms behind neurodegenerative diseases could revolutionize how we tackle these afflictions.
It’s also critical to note that the path to these discoveries was paved by curiosity-driven research, as highlighted by Stevens. The knowledge gained from her experiments with microglial cells demonstrates that even seemingly unrelated research can have profound implications for human health. Drawing connections between fundamental science and applied medicine fosters an environment where innovations in treating diseases can flourish. By continuing to support basic research, institutions can harness the potential of scientific inquiry to lead to pivotal breakthroughs in our strategy against Alzheimer’s and similar disorders.
Beth Stevens: A Pioneer in Alzheimer’s Research
Beth Stevens has gained recognition not only for her significant contributions to the understanding of microglial cells but also for her role in shaping the future of Alzheimer’s disease research. With her MacArthur ‘genius’ grant, she has secured a platform to advocate for and advance the study of the brain’s immune system, making her a key figure in neurology. Her insistence on the relevance of basic science illustrates how foundational studies can yield unexpected and valuable insights into the workings of complex brain disorders. Stevens’ work exemplifies how curiosity-driven research is fundamentally intertwined with potential therapeutic applications.
The impact of Stevens’ research transcends academic circles, resonating with families and individuals affected by Alzheimer’s disease. By investigating how abnormal microglial activity contributes to neurodegeneration, she is leading a charge towards more effective treatments and interventions. Stevens articulates a vision where understanding microglia not only enhances our biological knowledge but can also directly improve lives by informing healthcare strategies. This synergy between scientific inquiry and clinical relevance showcases a promising future in battling Alzheimer’s disease, transforming the way society approaches neurodegenerative diseases.
The Future of Alzheimer’s Disease Treatment
As the incidence of Alzheimer’s disease continues to rise, the urgency for effective treatments and preventative measures becomes dire. The research spearheaded by Beth Stevens and her team at Boston Children’s Hospital is paving the way towards innovative interventions that target the underlying mechanisms of the disease. Groundbreaking findings related to microglial cells and how they interact with neuronal networks may lead to novel pharmacological approaches that bolster neuroprotection. By addressing the immune system’s role in Alzheimer’s, researchers can potentially alter the disease’s trajectory before substantial cognitive decline occurs.
Moving forward, a focus on biomarkers for Alzheimer’s disease derived from microglial activity stands to revolutionize the detection and management of this debilitating condition. Enhanced diagnostic tools could lead to early interventions, which are crucial in managing neurodegenerative diseases. The integration of Stevens’ latest findings into clinical practice may offer hope for millions facing Alzheimer’s, turning the tide against a disease that has long been labeled as untreatable. Such an approach stresses the importance of continued investment in innovative research that bridges basic science and clinical application, ultimately improving care for those in need.
Challenges in Alzheimer’s Research
Despite the promising advancements in understanding Alzheimer’s disease, research faces several challenges. One major hurdle is the complexity of the disease itself, which is influenced by myriad genetic and environmental factors. The role of microglial cells adds another layer of complexity, as they can exhibit varied behavior based on context. For instance, while the activation of microglia can provide protective benefits, their overactivation can lead to inflammatory responses that damage neuronal health. This dual nature of microglial function necessitates a nuanced approach when developing therapeutic strategies aimed at combating neurodegeneration.
In addition to biological challenges, funding and resource allocation for Alzheimer’s research also present significant barriers. While support for neuroscience has increased, the demand for research far outweighs available funding, especially amid an aging population. Sustained federal funding, like that which supported Stevens’ early career, continues to be crucial for advancing research focused on Alzheimer’s and other neurodegenerative diseases. Robust funding not only facilitates groundbreaking studies but also ensures that discoveries are translated into effective clinical applications. Therefore, advocacy for ongoing financial support within the scientific community is essential.
Success Stories in Alzheimer’s Research
Highlighting success stories within Alzheimer’s disease research provides a sense of hope and motivation for scientists and families alike. One notable example is the progress made by Beth Stevens in understanding the role of microglial cells in neurodegeneration. Her findings have not only advanced our comprehension of the brain’s immune system but have also paved the way for new therapeutics. As researchers build on this foundational work, they are beginning to formulate treatment strategies that can tackle Alzheimer’s disease more effectively. This underscores the importance of ongoing research efforts in uncovering the mysteries surrounding neurodegenerative diseases.
Additionally, collaborative initiatives among research institutions and healthcare organizations have fueled advancements in early detection and intervention strategies for Alzheimer’s disease. By pooling resources and knowledge, scientists can leverage diverse expertise to develop comprehensive approaches. These collective efforts enhance the efficacy of studies related to biomarkers for Alzheimer’s and optimize treatment protocols that serve patients across different stages of the illness. Success in collaboration signifies a crucial step forward in the battle against neurodegenerative diseases, reinforcing the notion that progress is achievable through shared vision and commitment.
The Importance of Biomarkers for Alzheimer’s Disease
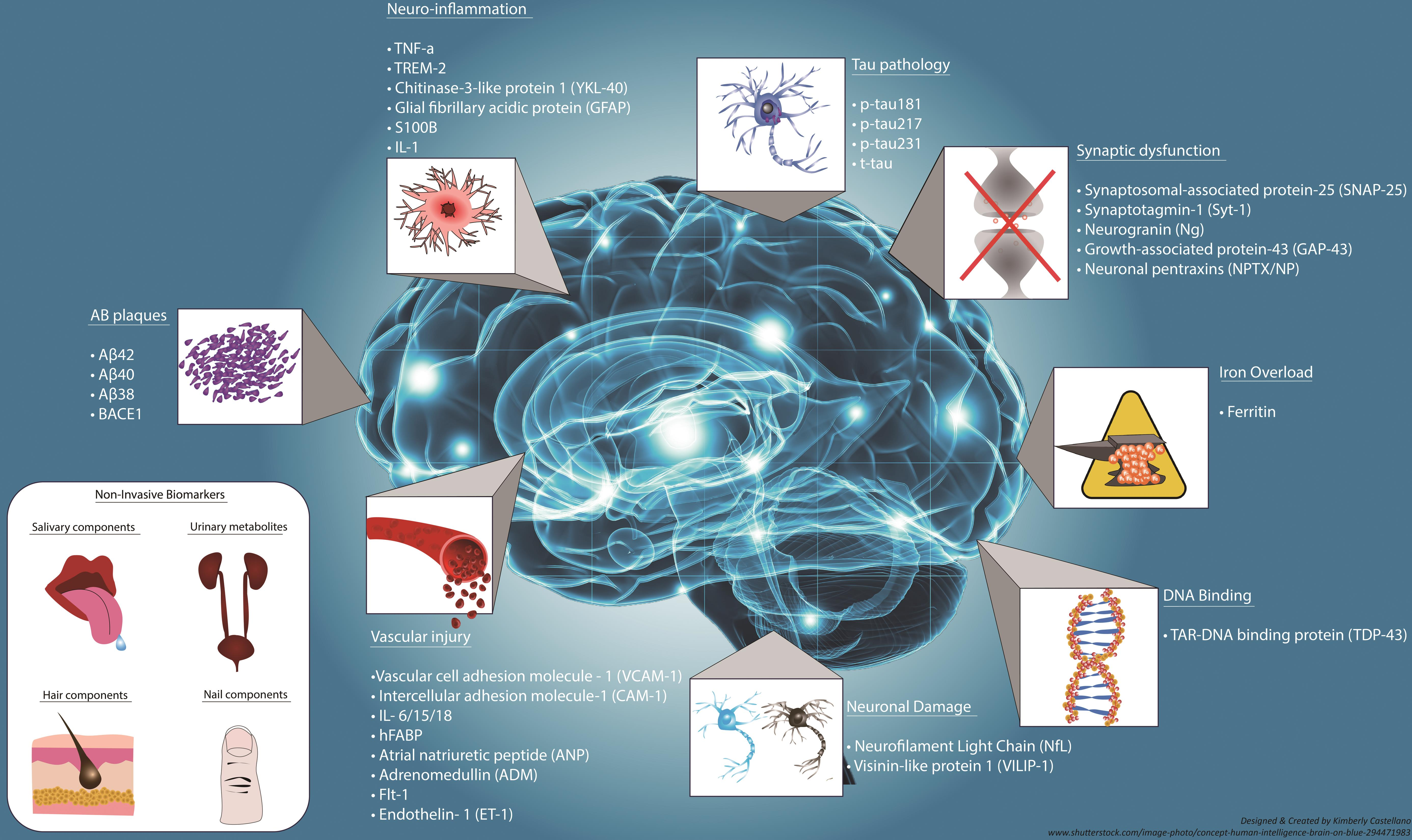
Biomarkers for Alzheimer’s disease are critical tools for diagnosing and monitoring disease progression, directly influencing treatment decisions. Stevens’ research emphasizes the potential to use microglial activity as a biomarker, providing early indicators that could signal the onset of the disease. Identifying these cellular markers can facilitate earlier interventions—an essential factor when considering the neurodegenerative nature of Alzheimer’s. With a better understanding of how microglial cells behave in response to Alzheimer’s pathology, new tests can be developed that offer greater accuracy in predicting and diagnosing the disease.
The integration of biomarkers into clinical practice represents a significant advancement in personalized medicine. As more tailored therapies are developed based on the behaviors identified through Stevens’ research, patients may receive more targeted care—allowing for adjustments to treatment plans that reflect individual responses to medications. This customization is invaluable for diseases with complex and varied presentations, like Alzheimer’s. As research evolves, the identification and validation of reliable biomarkers will undoubtedly enhance the clinical management of Alzheimer’s disease, ultimately improving patient outcomes.
The Interlink Between Microglia and Neurodegenerative Diseases
Recent advancements in the understanding of the interdependencies between microglial cells and neurodegenerative diseases have reshaped the landscape of Alzheimer’s research. The Stevens Lab has highlighted how microglia not only respond to injury but also play a critical role in shaping brain health and disease during aging. This represents a shift in perspective, acknowledging that rather than being passive bystanders, these brain immune cells actively engage in processes that may harm or protect neurodegenerative pathways. By studying these interactions, researchers can identify potential therapeutic targets that can either restore healthy microglial function or inhibit their detrimental activities.
Moreover, the implications of this research resonate across the spectrum of neurodegenerative diseases. Understanding the multifaceted role of microglia in Alzheimer’s may lead to breakthroughs in other conditions, such as Huntington’s or even Parkinson’s disease. The cross-pollination of knowledge across different fields of degenerative research fosters a collaborative spirit among neuroscientists aiming to unveil the complexities of brain disorders. This interconnected approach is vital for developing comprehensive strategies to combat neurodegeneration holistically, highlighting the importance of research that links microglia to a wider array of neurological conditions.
Funding and Support for Alzheimer’s Research Initiatives
Securing adequate funding for Alzheimer’s research initiatives is essential for expanding our knowledge and developing effective treatments. As noted by Beth Stevens, much of her work in understanding microglial cells and their role in neurodegenerative diseases was made possible through substantial government grants and support from entities like the National Institutes of Health (NIH). These resources not only enable researchers to conduct essential experiments but also encourage long-term studies that are crucial for yielding significant findings over time. As the urgency of Alzheimer’s disease continues to grow, sustained investment in research becomes increasingly critical.
The variability of funding sources can present challenges, as scientists navigate the complexities of grant applications and competition for limited resources. Advocacy for federal and state funding, alongside donations from private sectors, can create more robust mechanisms to support Alzheimer’s research. Collaborative funding efforts that unite research institutions, healthcare organizations, and philanthropists will foster an ecosystem where innovative ideas can thrive. This collective approach will enhance the overall progress in Alzheimer’s disease research, ensuring that vital questions are addressed and paving the way for transformative breakthroughs.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells serve as the brain’s immune system, playing a crucial role in Alzheimer’s disease research. They are responsible for removing damaged cells and pruning synapses, which is essential for healthy brain function. Research by scientists like Beth Stevens has demonstrated that faulty microglial pruning can lead to neurodegenerative diseases such as Alzheimer’s, highlighting the importance of these cells in developing new therapeutic strategies and understanding disease mechanisms.
How are biomarkers for Alzheimer’s disease discovered through research?
Biomarkers for Alzheimer’s disease are identified through extensive research into the biological processes underlying the disease. Studies like those conducted in Beth Stevens’ lab focus on neuroinflammation and microglial cell activity, leading to the identification of key biomarkers that can aid in early detection and monitoring of Alzheimer’s, ultimately improving patient outcomes.
What is Beth Stevens’ contribution to Alzheimer’s disease research?
Beth Stevens has significantly advanced Alzheimer’s disease research by uncovering the vital functions of microglial cells in the brain. Her findings regarding the role of these immune cells in synaptic pruning provide insights into how disruptions in this process can lead to neurodegenerative diseases like Alzheimer’s. Her work is paving the way for novel therapeutic approaches and biomarkers for early diagnosis.
Why is understanding the brain’s immune system important for tackling neurodegenerative diseases like Alzheimer’s?
Understanding the brain’s immune system, particularly through research on microglial cells, is crucial for addressing neurodegenerative diseases, including Alzheimer’s. This knowledge helps researchers grasp how immune responses contribute to neuronal health and disease progression, guiding the development of targeted therapies and prevention strategies that may slow or halt the progression of Alzheimer’s.
What impact does the aging population have on Alzheimer’s disease research?
The aging population significantly influences Alzheimer’s disease research, as the number of individuals affected by the disease is projected to double by 2050. Research efforts, such as those led by Beth Stevens, are increasingly focused on understanding the mechanisms of Alzheimer’s and developing effective treatments to manage the growing prevalence of this neurodegenerative condition.
How do federal funding and support contribute to Alzheimer’s disease research?
Federal funding, particularly from organizations like the National Institutes of Health, is vital for advancing Alzheimer’s disease research. This support enables scientists like Beth Stevens to explore fundamental questions about disease mechanisms, such as the role of microglial cells in neurodegenerative diseases. Continued investment in research is essential for discovering innovative treatments and understanding the complexities of Alzheimer’s.
What advancements have been made in Alzheimer’s disease research regarding therapeutic targets?
Recent advancements in Alzheimer’s disease research have identified microglial cells as potential therapeutic targets. Beth Stevens’ studies suggest that modulating the activity of these immune cells may lead to new treatment options that can alter the course of Alzheimer’s and other neurodegenerative diseases, offering hope for better management and prevention strategies.
What challenges exist in Alzheimer’s disease research that affect treatment developments?
Challenges in Alzheimer’s disease research include the complex nature of neurodegenerative processes and the difficulty in translating basic science findings into effective treatments. Despite breakthroughs, such as those related to microglial cells and biomarkers, researchers like Beth Stevens emphasize the need for continued funding and support to overcome these hurdles and improve therapeutic interventions.
| Key Point | Details |
|---|---|
| Microglial Cells | Act as the brain’s immune system, removing dead cells and pruning synapses. |
| Impact on Alzheimer’s Disease | Faulty pruning by microglial cells may contribute to Alzheimer’s and other neurodegenerative disorders. |
| Research Contributions | The Stevens Lab’s discoveries pave the way for new medications and biomarkers for early detection. |
| Funding Sources | Research supported by National Institutes of Health and federal funding. |
| Future Projections | The incidence of Alzheimer’s is expected to double by 2050, raising care costs significantly. |
Summary
Alzheimer’s disease research is critical in understanding and addressing the growing challenge of neurodegenerative disorders. Neuroscientist Beth Stevens has made significant strides in revealing the role of microglial cells in the brain, linking their malfunction to conditions like Alzheimer’s disease. Her groundbreaking work is not only vital for developing effective treatments but also for identifying early biomarkers that can lead to timely interventions. With the number of Alzheimer’s cases projected to rise dramatically in the coming decades, continued investment in such research is essential for enhancing the quality of life for millions.