Maternal mortality rates in the United States remain alarmingly high, with over 80% of pregnancy-related deaths deemed preventable. This troubling statistic underscores the urgency for renewed focus on improving maternal health disparities across various demographics. According to recent studies, the U.S. has the highest maternal mortality rate among high-income countries, which has only increased between 2018 and 2022. Key culprits contributing to these preventable deaths include inadequate postpartum care and escalating chronic conditions like cardiovascular disease among new mothers. Addressing these issues is not only crucial for the well-being of mothers but also for the health of future generations.
The issue of maternal mortality captures the gravity of pregnancy-related fatalities and emphasizes the need for effective healthcare reforms. Pregnancy-associated deaths have become a critical public health challenge, with widening health inequities revealing alarming trends among racial and ethnic minorities. Late maternal mortality—deaths occurring after the immediate postpartum phase—has also raised concerns about continuity in care beyond the traditional six-week postpartum window. As chronic conditions, such as cardiovascular issues, affect younger populations more than ever before, it is vital to re-evaluate our approach to postpartum healthcare policies. By aligning resources and strategies that cater to the specific needs of mothers in diverse communities, we can aim to diminish these preventable deaths and promote healthier outcomes for all.
Understanding Maternal Mortality Rates in the U.S.
The persistent issue of maternal mortality rates in the United States is alarming, as the nation consistently records the highest rates among high-income countries. Recent data reveals that more than 80 percent of pregnancy-related deaths are preventable, yet disparities based on race, state, and healthcare access continue to drive these tragic outcomes. For example, American Indian and Alaska Native women face mortality rates nearly four times higher than those of their white counterparts, highlighting significant maternal health disparities that require urgent attention and action.
Factors contributing to these elevated rates are multifaceted, including a fragmented healthcare system, inequitable policies, and chronic health issues exacerbated by systemic bias. Notably, cardiovascular diseases have become a leading cause of maternal mortality, indicating a troubling trend of young individuals developing chronic conditions such as hypertension. To address these preventable deaths and improve maternal health outcomes, extensive reforms in healthcare infrastructure and policies, especially concerning prenatal and postpartum care, are essential.
Preventable Deaths and Their Impact on Maternal Health
Preventable deaths among pregnant individuals underscore a critical public health challenge in the U.S. The transition of leading pregnancy-related deaths from hemorrhage to cardiovascular disease serves as a stark reminder of the changing landscape of maternal health. The rise in chronic conditions like hypertension among younger women poses serious concerns, suggesting that the focus on immediate postpartum care may be insufficient without addressing these underlying health issues.
Moreover, understanding and improving the continuum of care from pregnancy through the extended postpartum period could significantly reduce late maternal deaths, which often go unreported. The inclusion of these late maternal deaths in the broader conversation about pregnancy-related mortality can encourage a more holistic approach to maternal healthcare, ensuring that policies not only cover initial postpartum periods but also provide adequate support throughout the entire year, thus reducing preventable deaths.
Another vital aspect of addressing preventable deaths lies in tackling healthcare disparities that disproportionately affect minority and underserved populations. Implementing targeted interventions and resources can help minimize barriers such as access to quality prenatal care and postpartum services. With the United States leading high-income nations in maternal mortality rates, focusing on preventable deaths through public health initiatives and policies is a necessary step towards ensuring the safety and well-being of mothers.
Racial Disparities in Maternal Health Outcomes
Racial disparities in maternal health outcomes present a stark reality that must be addressed in the fight against high maternal mortality rates. Studies indicate that American Indian, Alaska Native, and Black women experience significantly higher rates of maternal mortality compared to their white counterparts. These disparities are rooted in systemic inequalities within the healthcare system, including bias, lack of access to care, and social determinants of health that disproportionately affect these communities.
To combat this injustice, it is crucial to implement policies that promote equity in maternal healthcare, such as expanding access to prenatal and postpartum services to marginalized groups. Public health initiatives aimed at educating healthcare providers on culturally competent care can also help reduce biases that contribute to poor maternal health outcomes. By acknowledging and addressing these racial disparities, the U.S. can work towards a future where all individuals have the same chances of safe and healthy pregnancies.
The Role of Postpartum Care in Maternal Health
Postpartum care plays a pivotal role in safeguarding maternal health and reducing mortality rates. Recent studies have shown that a significant percentage of pregnancy-related deaths occur beyond six weeks postpartum, indicating the necessity of extending care into the first year after childbirth. However, many healthcare systems are inadequately designed to provide comprehensive support during this crucial period.
To improve outcomes, healthcare providers must adopt a more inclusive approach that recognizes the postpartum period as an extended continuum rather than a discrete timeframe. Enhancing postpartum care protocols to include regular check-ups and screenings for conditions such as cardiovascular disease can significantly reduce mortality rates and improve maternal health. This paradigm shift is essential for addressing the alarmingly high rates of preventable deaths experienced in the U.S.
Investing in Maternal Health Infrastructure
The recent rise in maternal mortality rates signals a dire need for increased investment in maternal health infrastructure. With the assertion that over 80 percent of pregnancy-related deaths are preventable, it becomes imperative to allocate resources toward improving quality of care during pregnancy and expanding supportive services in the postpartum period. A robust public health framework can ensure that all women, regardless of their backgrounds, receive quality maternal care.
Furthermore, states must recognize and address the variability in maternal health outcomes by implementing evidence-based policies that target high-risk populations and regions. States that exhibit lower rates of maternal mortality, such as California, provide valuable insights into successful strategies that can be replicated nationally. By prioritizing maternal health and investing in comprehensive healthcare solutions, the U.S. can aim to reduce preventable deaths to align more closely with the standards of other high-income countries.
The Impact of Chronic Health Conditions on Maternal Mortality
The rising prevalence of chronic health conditions, particularly cardiovascular disease, among pregnant individuals poses a significant risk to maternal health. As chronic conditions like hypertension increasingly affect younger populations, there is a critical need to address how these diseases contribute to pregnancy-related mortality. Understanding the interplay between pre-existing conditions and pregnancy can guide clinicians in providing the necessary interventions for at-risk women.
Effective management of such health challenges must begin prior to pregnancy, focusing on education and prevention strategies that empower individuals to maintain their health. Integrating routine cardiovascular assessments into prenatal care can help identify risks early, improving care and outcomes. By prioritizing the management of chronic health conditions, healthcare providers can play a crucial role in reducing maternal mortality and enhancing overall maternal health.
Policies to Mitigate Maternal Health Disparities
Creating effective policies to mitigate maternal health disparities is essential in addressing the rising maternal mortality rates in the U.S. Legislative measures that ensure equitable access to quality healthcare can provide underserved populations with the support they need during and after pregnancy. Policies that promote comprehensive insurance coverage for prenatal and postpartum services can help alleviate the financial barriers that often deter women from seeking care.
Moreover, community outreach programs that focus on educating marginalized populations about their maternal health rights can empower individuals to advocate for their needs. Collaborating with local organizations and healthcare providers to develop culturally tailored programs can further enhance engagement and care uptake. By addressing the systemic injustices in maternal care, we can foster an environment where every woman has fair access to the quality services they deserve regardless of their racial or socio-economic background.
The Need for Comprehensive Maternal Health Research
The limitations of current maternal health research highlight the urgent need for a comprehensive approach to studying maternal mortality rates. Historically, inconsistent tracking and reporting practices have hampered the effectiveness of data-driven strategies aimed at reducing pregnancy-related deaths. By establishing a national registry for maternal deaths, healthcare systems can gain a clearer understanding of the factors contributing to these deaths and develop targeted interventions.
Additionally, funding for maternal health research must be prioritized to explore the multiple dimensions of maternal health, including chronic conditions, access to care, and social determinants. Research that encompasses diverse populations and examines the impact of maternal experiences can inform policy development and improve health outcomes. With robust research efforts, the U.S. can begin to uncover solutions necessary for reducing maternal mortality and advancing the health of all mothers.
Strengthening Community-Based Maternal Health Programs
Community-based maternal health programs are crucial in addressing the social determinants that contribute to maternal mortality rates. By focusing on the specific needs and challenges faced by women in their locales, these programs can offer tailored services that directly respond to maternal health disparities. Initiatives that involve community health workers can bridge the gap between healthcare systems and underserved populations, providing essential support and education.
Furthermore, integrating maternal health services with broader community resources, such as housing assistance and nutrition programs, can create a more holistic support system for pregnant individuals. This multifaceted approach can enhance maternal care quality, improve health outcomes, and ultimately reduce the incidence of preventable deaths. Investing in community-based solutions is a vital step in ensuring that all women receive the comprehensive care they need throughout their pregnancy journeys.
Frequently Asked Questions
What are maternal mortality rates and how do they relate to pregnancy-related deaths?
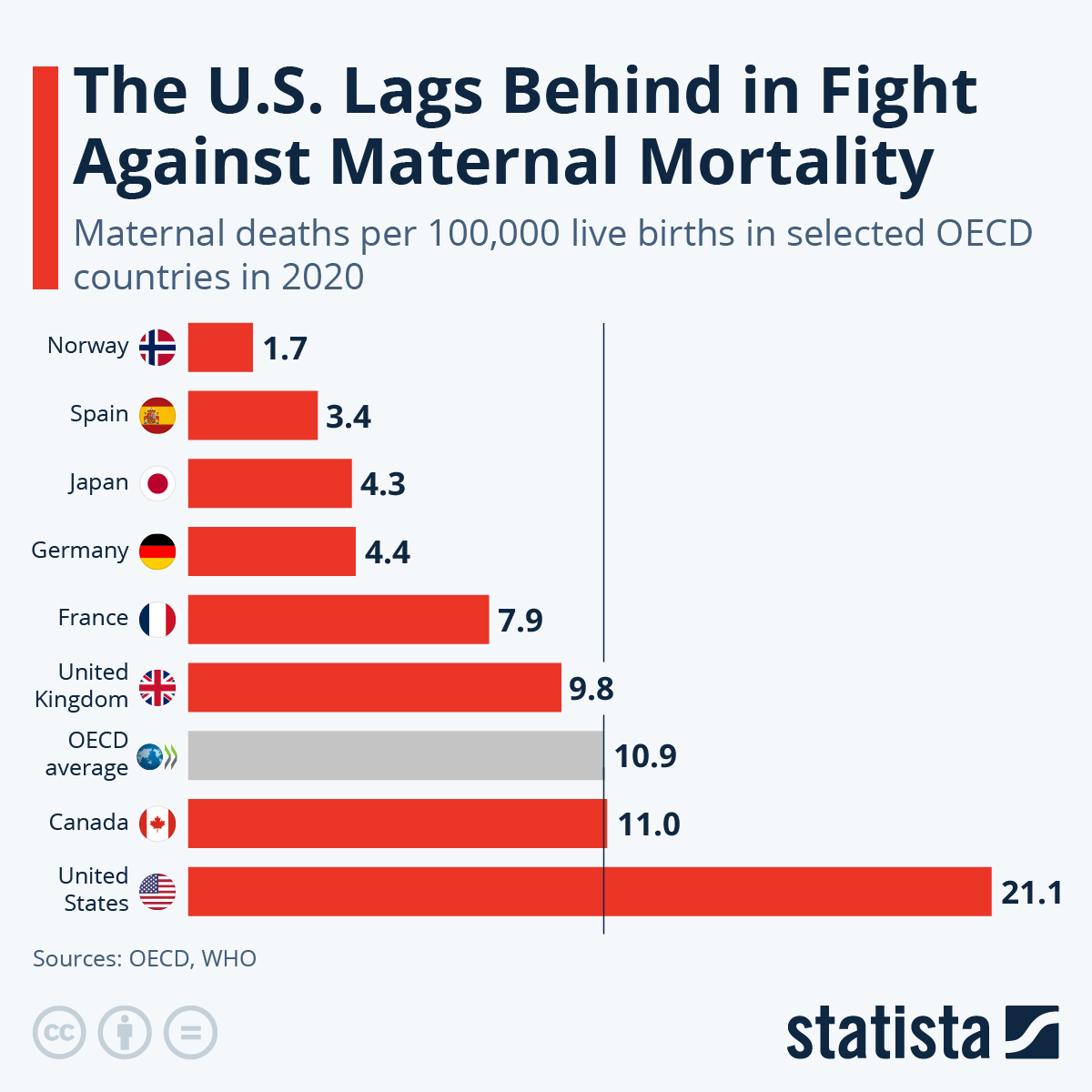
Maternal mortality rates refer to the number of pregnancy-related deaths occurring per 100,000 live births. In the U.S., many of these deaths are preventable, highlighting significant issues in maternal healthcare and disparities in outcomes.
Why are maternal mortality rates in the U.S. rising despite being a high-income country?
The rise in U.S. maternal mortality rates is attributed to factors such as a fragmented healthcare system, inequitable policies, and increasing rates of chronic conditions like cardiovascular disease among pregnant individuals, which pose risks during and after pregnancy.
How do racial disparities affect maternal mortality rates in the U.S.?
Racial disparities significantly impact maternal mortality rates, with American Indian, Alaska Native, and non-Hispanic Black women experiencing much higher rates compared to white women. Ongoing systemic bias and a lack of equitable healthcare contribute to these alarming differences.
What role does postpartum care play in reducing maternal mortality rates?
Improving postpartum care is crucial as nearly a third of pregnancy-related deaths occur between 42 days to 1 year after childbirth. A more comprehensive approach to postpartum care can help address long-term health issues and reduce maternal mortality rates.
How does cardiovascular disease impact maternal health and mortality rates?
Cardiovascular disease has emerged as the leading cause of pregnancy-related deaths in the U.S., accounting for over 20% of such fatalities. The increasing prevalence of chronic hypertension in younger populations is raising concerns regarding maternal health outcomes.
Why should late maternal deaths be included in maternal mortality rate calculations?
Including late maternal deaths—those occurring between 42 days and 1 year post-pregnancy—in mortality statistics is vital as it emphasizes the importance of continuous healthcare support postpartum, beyond the traditional six-week checkup.
What can be done to lower maternal mortality rates in the U.S.?
To combat rising maternal mortality rates, the U.S. must invest in public health infrastructure, improve access to quality prenatal and postpartum care, and address policy disparities at state levels to ensure equitable healthcare for all pregnant individuals.
What are the implications of rising maternal mortality rates for maternal health disparities?
The rise in maternal mortality rates exacerbates existing maternal health disparities, revealing a critical need for effective interventions and policy changes to ensure equitable health outcomes, especially among marginalized communities.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, with rates rising from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, emphasizing the need for better healthcare systems. |
| Disparities in Maternal Mortality | Significant racial disparities exist, with American Indian and Alaska Native women experiencing the highest mortality rates. |
| Leading Causes of Maternal Death | Cardiovascular disease is the leading cause, accounting for over 20% of deaths, and rising rates of hypertension in younger women are noted. |
| Need for Policy Changes | The study suggests that states can improve outcomes by learning from those with lower rates, like California. |
| Importance of Extended Postpartum Care | Late maternal deaths (those occurring within a year after pregnancy) account for a significant portion of maternal mortality, highlighting the need for better healthcare beyond six weeks postpartum. |
Summary
Maternal mortality rates in the United States are a pressing public health issue that continues to rise, highlighting systemic health disparities and the need for immediate action. A recent study reveals alarming trends, with significant increases in pregnancy-related deaths, especially among marginalized racial groups. By understanding the critical factors contributing to these rates, such as preventable causes and the need for comprehensive postpartum care, stakeholders can push for essential policy changes that prioritize maternal health equity. Emphasizing the importance of investing in public health infrastructure is crucial for reversing these trends and ensuring that all women receive the quality care they deserve throughout their pregnancy journey.