Medical research funding plays a crucial role in advancing healthcare and ensuring patient safety in research. With grants from institutions like the NIH, researchers can conduct extensive studies that follow strict ethical guidelines, including the oversight provided by Institutional Review Boards (IRBs). These boards are pivotal in reviewing research proposals to safeguard participant rights and well-being, making the implications of funding cuts particularly concerning. A reduction in financial support jeopardizes not only the progress of vital medical studies but also the integrity of clinical trials that rely on collaborative efforts across multiple sites. As funding sources dwindle, the potential risks faced by study participants and the broader healthcare landscape become alarmingly pronounced.
In the realm of healthcare innovation, financing for scientific inquiries is indispensable for driving forward effective medical solutions. Allocations of research capital, particularly from government entities like the National Institutes of Health (NIH), facilitate rigorous investigations that uphold patient rights and safety. Oversight mechanisms, such as the role of IRBs in overseeing clinical investigations, ensure ethical compliance and participant protection. However, diminishing resources pose a significant risk to the sustainability of such safeguards, ultimately affecting trust in medical research. Consequently, the issue of funding cuts not only impacts the immediate research environment but also reverberates through collaborative health studies, compromising the well-being of individuals participating in these essential trials.
The Importance of Medical Research Funding
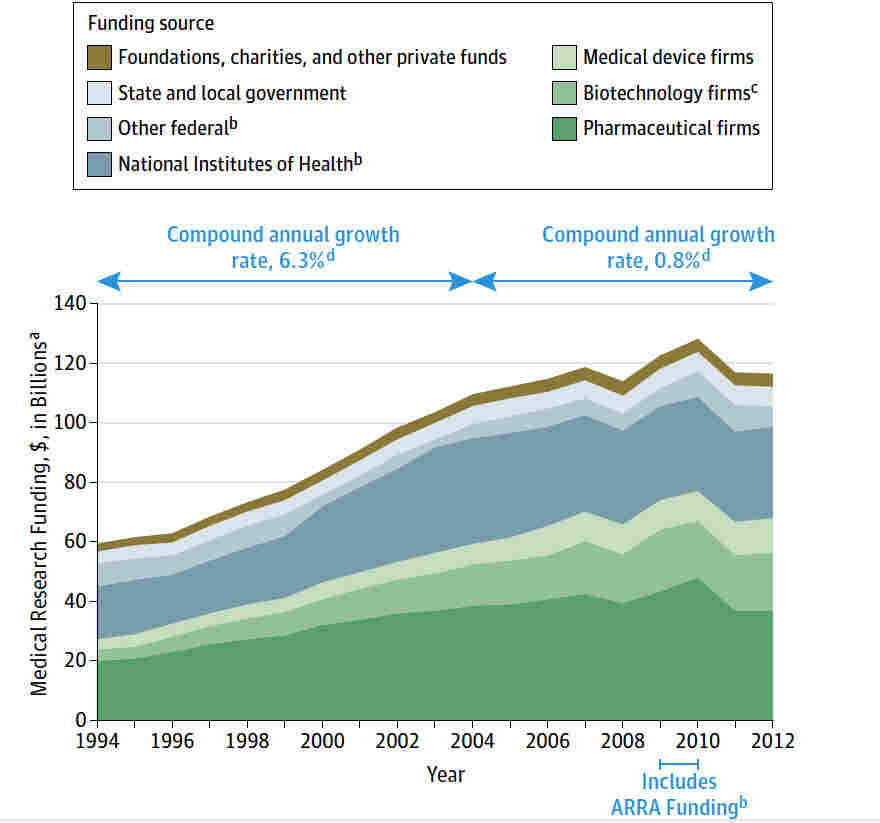
Medical research funding is essential for advancing healthcare and ensuring patient safety. It provides the necessary resources for conducting rigorous scientific studies, developing new treatments, and improving patient care protocols. When adequate funding is available, researchers can investigate innovative solutions and implement trials aimed at preventing diseases. However, when research funding is curtailed, as seen with the recent cuts impacting institutions like Harvard, the implications can be dire, jeopardizing vital research initiatives and, ultimately, patient welfare.
The National Institutes of Health (NIH) play a significant role in supporting medical research through grants that enable institutions to carry out their studies. Such funding not only promotes groundbreaking biomedical discoveries but also ensures compliance with ethical guidelines to protect participants. Reduced funding might lead to a high-pressure environment where essential aspects of patient safety get overlooked in an attempt to cut costs, thereby increasing the risks associated with clinical trials and diminishing public trust in medical research.
Impact of Funding Cuts on Patient Safety
Funding cuts can have a profound impact on patient safety in clinical studies. With fewer resources available, research institutions may struggle to adhere to the rigorous standards set forth by Institutional Review Boards (IRBs), which oversee research protocols to protect participants. This oversight is critical to ensuring that potential risks are evaluated and that ethical standards are maintained throughout the research process. We’re witnessing firsthand how these funding disruptions can jeopardize the very framework designed to protect volunteers in clinical studies.
When funding is halted, as seen with the SMART IRB system, ongoing studies face significant delays, and new clinical sites cannot join research initiatives. This not only affects the integrity of the research but also poses risks to patient safety. Participants may be left without necessary supervision or support, making it difficult to manage adverse effects or complications that arise during trials. Therefore, it’s crucial for policymakers to recognize the importance of sustained funding in maintaining both innovation in medical research and the safety of its participants.
The Role of IRBs in Safeguarding Research Participants
Institutional Review Boards (IRBs) are integral to ensuring the safety and ethical treatment of individuals participating in clinical research. They meticulously review study designs and monitor compliance with ethical standards, ensuring participants are informed about potential risks and benefits of their involvement. By implementing thorough review processes, IRBs help foster trust between research institutions and participants, crucial for successful recruitment and retention in studies.
Furthermore, while IRBs operate independently, their collaboration with funding agencies like the NIH is essential for protecting patient safety in research. They provide a system of checks and balances, addressing historical ethical breaches that have undermined public confidence in clinical research. With funding cuts threatening IRB operations, the risk of lapses in ethical standards and participant oversight increases, potentially leading to negative consequences for researchers and communities involved.
Collaborative Medical Studies: What’s at Stake?
Collaborative medical studies represent a critical approach to conducting research that brings together various institutions to pool resources, expertise, and data. This model enhances the scope and scale of research while allowing for quicker and more efficient testing of new interventions. However, when government funding is trapped in bureaucratic hurdles, like the recent halting of SMART IRB funding, many collaborative efforts are stalled, limiting the potential for significant medical advancements that could benefit the larger population.
In addition, such funding disruptions can hinder the momentum of groundbreaking studies. They require various sites functioning together seamlessly, which cannot happen if financial resources are restricted. This not only affects the research at hand but can also lead to a long-term downturn in collaborative efforts, dissuading researchers from working across institutions due to fear of uncertainty. The costs of such stagnation are ultimately borne by patients who might miss out on innovative treatments that required a collaborative effort to develop.
Understanding the Long-term Consequences of Research Funding Cuts
The consensus among medical professionals is that the long-term consequences of funding cuts in research will be detrimental not just to immediate studies but also to broader public health initiatives. Historical context illustrates that diminished investment in healthcare research hampers scientific progress, leading to a backlog of critical investigative work. This could mean longer waits for new drug approvals, fewer innovations, and ultimately, a rise in preventable diseases as available treatments lag behind demand.
Moreover, when research funding is compromised, it fosters a cycle of mistrust among community members who may feel that their safety is being sacrificed for the sake of budgetary constraints. This erosion of trust can discourage participation in clinical studies, furthering the challenges that researchers face in recruiting volunteers for essential trials. Moving forward, it’s vital that advocacy for medical research funding incorporates the importance of preserving patient safety and community trust at its core.
Building Public Trust Through Transparent Funding
To maintain public trust, transparency in how medical research funding is allocated and utilized is crucial. Communities must believe that their safety is prioritized in clinical trials, which necessitates clear communication about how funds are being used to uphold ethical standards. Research institutions must demonstrate accountability in their financial practices, showcasing how every dollar contributes to patient safety and institutional integrity.
Engaging communities in dialogue about research funding can help bridge the gap between researchers and the public. By clearly outlining the impact that funding has on ensuring safety in clinical studies, institutions can cultivate a more informed population, eager to participate in research endeavors. This two-way engagement enhances trust and fosters collaboration, benefiting all stakeholders involved.
Addressing Historical Ethical Issues in Medical Research
Historical events have underscored the need for strict ethical oversight in medical research. The traumatic legacy of studies that exploited vulnerable populations has led to the establishment of systems like IRBs that are dedicated to protecting research participants. However, as funding cuts threaten these safeguards, there exists a risk of regression to less stringent oversight behaviors that could re-open old wounds related to public trust.
To counteract this risk, ongoing education and training in ethics for researchers and IRB members are essential. Furthermore, adequate funding is necessary to support these educational initiatives and ensure that research ethics are placed at the forefront of all clinical studies. Institutional commitment to ethical oversight can help address past injustices while guarding against future ethical lapses in the research landscape.
The Future of Patient-Centric Research
The future of patient-centric research hinges significantly on the availability of robust funding and the support of multi-site collaborative studies. As the landscape of medical research evolves, it is essential to integrate patient feedback into the research process actively. This approach promotes a sense of ownership among participants and helps researchers design studies that are more aligned with patient needs and safety.
Moreover, fostering collaborations between researchers, clinicians, and the community enhances the delivery of more effective, patient-centered care. Researchers should strive to include diverse populations in clinical trials to ensure that findings can benefit the wider community. A commitment to inclusive research practices, supported by adequate funding, is paramount for translating results into tangible health outcomes that resonate with patients’ lived experiences.
Legislation’s Role in Research Funding and Patient Safety
Legislation plays a pivotal role in securing the funding necessary for safe and effective medical research. Policies enacted at both the federal and state levels can determine the flow of funds to research institutions and ultimately influence the scope of patient safety measures that are implemented. Legislative support for NIH funding is critical, as these funds underlie the infrastructure that governs medical research initiatives.
Furthermore, lawmakers need to work closely with research institutions and advocacy groups to ensure that funding policies reflect the pressing needs of medical research and patient safety. Without the support of policy decisions and advocacy, the risk of significant funding cuts will continue to pose a threat to the integrity of research and the protection of participants who volunteer for clinical studies.
Frequently Asked Questions
How does medical research funding impact patient safety in clinical trials?
Medical research funding plays a crucial role in ensuring patient safety during clinical trials. Adequate funding allows for comprehensive oversight by Institutional Review Boards (IRBs), which review and approve research protocols to protect participants’ rights, safety, and welfare. When funding cuts occur, as seen with significant reductions in NIH research grants, the ability of IRBs to effectively monitor trials diminishes, potentially jeopardizing patient safety.
What is the role of IRBs in ensuring the ethical conduct of medical research?
IRBs, or Institutional Review Boards, are integral to the ethical conduct of medical research. They review study proposals to ensure participant safety, evaluate the method of informed consent, assess risks, and monitor ongoing trials. This oversight is particularly essential in collaborative medical studies requiring multiple institution involvement, as stipulated by NIH rules that mandate a single IRB (sIRB) approach. Recent funding cuts threaten the resources available for IRB operations, thereby affecting the oversight necessary to protect study participants.
What are the potential consequences of funding cuts for medical research?
Funding cuts can lead to halted or delayed medical research studies, compromising the safety and welfare of participants involved. As observed with the stoppage of over $2 billion in federal research funds, these cuts disrupt ongoing studies and collaboration across institutions, damaging public trust in the research community. Furthermore, inadequate funding limits an IRB’s capacity to enforce ethical standards, ultimately risking the integrity of clinical trials and patient safety.
How do NIH research grants contribute to advancing patient safety?
NIH research grants are vital for supporting comprehensive safety measures in clinical trials. These grants finance key activities such as IRB reviews and monitoring systems that safeguard participant welfare. Without robust funding from NIH grants, the ability to conduct thorough IRB assessments is jeopardized, which can lead to insufficient safety protocols in medical studies, particularly those involving vulnerable populations.
In what ways can collaborative medical studies enhance patient safety?
Collaborative medical studies enhance patient safety by pooling resources, expertise, and best practices across multiple institutions. This teamwork often involves shared oversight by a single IRB, which streamlines processes and improves monitoring of participant welfare. However, the interruption of funding can hinder collaborative efforts, limiting the effectiveness of such studies in ensuring rigorous safety standards and ethical conduct.
What are the implications of a stop-work order on medical research funding?
A stop-work order, such as the one affecting SMART IRB, stops new clinical sites from participating in ongoing studies and delays vital research efforts. This directly impacts patient safety by halting oversight processes and can exacerbate public mistrust in medical research, creating additional barriers for investigators and institutions to conduct ethical and safe studies.
| Key Point | Details |
|---|---|
| Funding Cuts Impact | The Trump administration’s freeze of over $2 billion in federal research grants to Harvard disrupts patient safety efforts in medical research. |
| SMART IRB’s Role | The SMART IRB system, managed by Harvard Catalyst and collaborators, facilitates oversight across multiple research sites. |
| Importance of IRBs | Institutional Review Boards ensure compliance with regulations and protect the rights and welfare of research participants. |
| IRB Responsibilities | IRBs review research proposals, ensure informed consent, assess risks, and provide training to investigators to maintain ethical standards. |
| Historical Context | The establishment of IRBs was a response to historical ethical breaches in research, such as the Tuskegee Syphilis Study. |
| Current Funding Crisis | The stop-work order has halted ongoing studies, preventing the addition of new sites and causing significant delays and risks to patient safety. |
| Need for Continued Support | Despite funding cuts, Harvard Medical School provides support to maintain collaborative research and safeguard public health. |
Summary
Medical research funding is essential for ensuring patient safety and the integrity of research practices. The recent cuts to funding have posed serious risks not just to ongoing studies but also to the trust between researchers and the communities they serve. As highlighted, the role of Institutional Review Boards (IRBs) is critical in monitoring and safeguarding the rights of participants. Continued advocacy for medical research funding is vital to uphold ethical standards and protect public health.